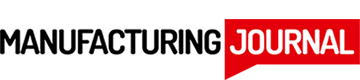
It takes months of research and development and thousands of people to bring new medicines from the lab to shelves. Researchers and drug developers use a rigorous process of medical investigation, testing and review to identify and test new medicines. This process starts with insightful medical research.
1. Preliminary Research
At the first stage in the development of any new medicine, researchers are focused on learning more about a certain disease, medical condition or illness in need of better treatment options. Preliminary research often takes place in academic settings, where initial discoveries and theories are explored without plans to develop or market an actual treatment.
Preliminary research involves investigating a medical condition and identifying features that could be useful for developing new treatments. For instance, researchers might notice that a certain protein could weaken a harmful virus. Researchers publish their findings for other members of the scientific community to use.
2. Treatment Discovery
Leads uncovered in preliminary research may spark inspiration for a possible treatment method. This begins the second stage of a medicine’s journey to market — treatment discovery. The treatment discovery process usually involves testing many possible treatments, such as different proteins or chemical compounds. Thousands of initial candidates may be screened.
The treatment discovery process has experienced some exciting innovations in recent years. Researchers have developed AI machine learning algorithms that can automate the process of screening chemical compounds or molecules for potential medical uses. Industry leaders estimate that AI drug discovery could significantly reduce development time for new treatments.
Manually testing thousands of possible treatments could take years. AI automates most of the process, narrowing it down to the most promising candidates. Then, researchers can look more closely at the initial pool of candidates and identify those with the best potential for being effective.
3. Testing Treatment Candidates
The next stage of medicine development is all about testing and refining the treatment candidates. At this stage, researchers usually have a pool of about 10-20 “finalist” candidate treatments. They’re focused on developing theories into actual products that could potentially move on to clinical trials.
While there are many methods for testing different treatment candidates, researchers usually have similar goals. At this stage, they’re focused on efficacy and safety. Researchers often use computer models to run preliminary tests and refine treatment candidates. The results of these tests help alter treatment candidates to make them safer and more effective for patients.
For example, researchers may test out different particle size distributions, which impacts how easy a drug is to digest and how it affects the patient’s digestive system. Particle size distribution can also impact the safe dosage of the treatment and the manufacturing process needed to produce it.
4. Approval and Review
Once researchers have a few promising treatment candidates, they can apply for approval and medical review. This step is crucial for moving on to clinical trials. Official medical and scientific boards will review the research and development behind the treatment so far to confirm it has been thoroughly tested for safety and efficacy.
In the U.S., the main body responsible for reviewing and approving new drugs is the Food and Drug Administration (FDA). The Center for Drug Evaluation and Research has a 12-step process for obtaining full FDA approval. This process begins with initial development and testing, then an investigational new drug (IND) application. This application is the first round of formal review by the FDA. Only after the IND review can drug developers move on to clinical trials.
5. Clinical Trials
Clinical trials are the proving ground where developers find out if their new treatment is actually effective or not. Prior to this stage, they may have conducted animal and virtual model testing, but no humans have tried the new treatment yet.
There are multiple stages of clinical trials. The first usually starts with 20-80 volunteers. Proper screening ensures that clinical trials are safe and effective for everyone involved. Researchers will initially stick to a specific demographic of patients and require certain health standards. A wider range of patients can be invited to clinical trials as the medicine advances to later trial stages.
Technology is increasingly helping treatment developers in clinical trials. AI can help screen clinical trial patients by using their electronic health records to predict possible medical complications. AI algorithms are great at pattern recognition, making them perfect for repetitive tasks like scanning medical records. These abilities help treatment developers conduct clinical trials more efficiently and get new treatments to market sooner.
Treatment developers usually go through at least three clinical trial stages. By the time clinical trials are concluded, thousands of patients have tested the new treatment. If it has proven safe and effective, the new medicine can move on to the last stage of its journey.
6. Authorization and Patenting
Next, treatment developers meet with the FDA again to review the results of clinical trials. This is the final review stage to ensure the findings are legitimate. Once officials from the FDA review all of the data and determine that it is safe for sale in the U.S., they will approve the new drug application (NDA) for the product.
Once a treatment has FDA approval, the developer also needs to patent it. Bringing new medicines from R&D to market can cost hundreds of millions of dollars — some even go upwards of $4 billion dollars.
With the new treatment approved and patented, it’s ready to go into production. Doctors can use the new treatment to help thousands of patients live healthier lives.
The Journey From the Lab to Patients
Bringing a new medicine to market requires extensive research and investigation from scientists and doctors. It costs millions of dollars and requires months or years of hard work to bring a new medical treatment from the lab to patients. Technology can help scientists make the process more efficient so people get the life-saving treatments they need sooner.